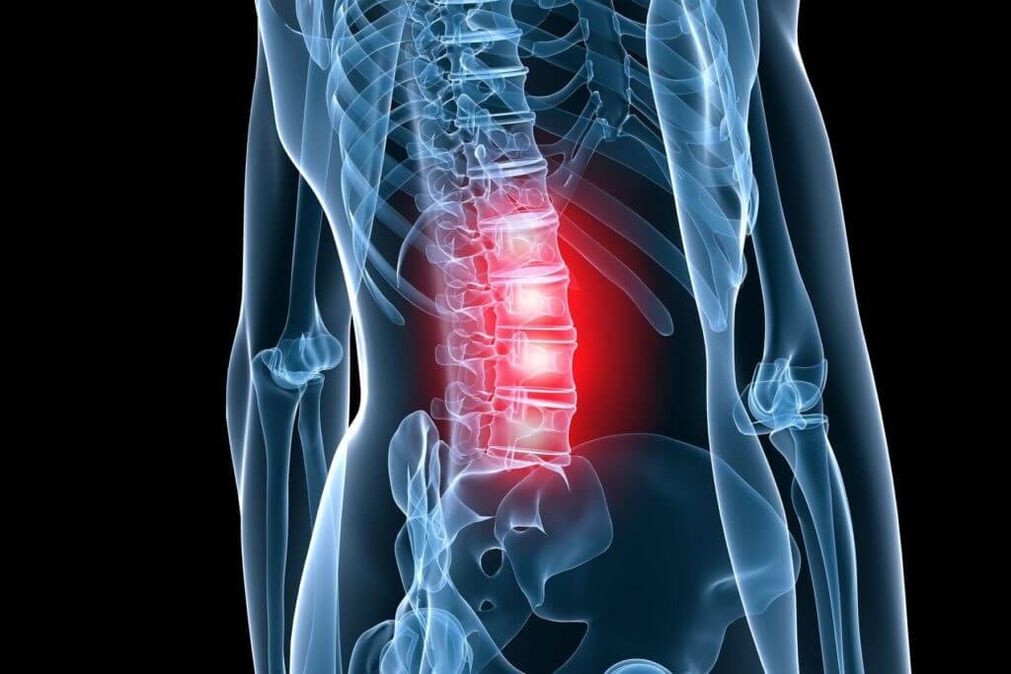
painin the back is a at least once in a lifetime experience for 4 out of 5 people. As for the working population, theyMost common cause of disabilitythis determines their economic and social importance in all countries of the world. Among the diseases accompanied by pain in the lumbar spine and extremities, one of the main sites of bone necrosis.
Osteochondrosis of the spine (OP) is a degenerative-dystrophic lesion that begins in the medullary nucleus of the disc and extends to the annulus and other elements of the spinal segment with frequent secondary effects on the spine. adjacent neural circuit formations. Under the influence of unfavorable static-dynamic loads, the elastic colloidal nucleus (glue) loses its physiological properties - it dries out and sequesters over time. Under the action of mechanical load, the fibrous ring of the disc, losing its elasticity, protrudes, and subsequently, fragments of the pulp nucleus fall out through its cracks. This leads to the appearance of acute pain (low back pain), because. Peripheral parts of the annulus contain receptors of the Luschka nerve.
Stages of osteonecrosis
The visceral pathological process corresponds to stage 1 (period) (OP) according to the classification proposed by Ya. Yu. Popelyansky and A. I. Osna. In the second period, not only the amortization capacity was lost, but also fixed functionality with the development of hyper-portability (or instability). During the third period, the formation of a herniated (convex) disc is observed. According to their degree of prolapse, herniated discs are divided intoelastic convexwhen there is uniform protrusion of the disc, andisolated protrusion, characterized by irregular and incomplete rupture of the annulus. The nucleus pulposus migrates into these ruptures, creating localized protrusions. With a partially prolapsed disc herniation, all the capsular layers are ruptured, possibly ruptured the posterior longitudinal ligament, but the disc protrusion itself has not lost contact with the central nucleus. Complete prolapsed disc herniation means that not individual pieces of it, but the entire nucleus, prolapse into the lumen of the spinal canal. According to the diameter of disc herniation, they are divided into foraminal, posterol edge, paramedian and median. The clinical manifestations of disc herniation are diverse, but it is at this stage that various compression syndromes often arise.
Over time, the pathological process can migrate to other parts of the spinal motor segment. The increased load on the vertebral bodies leads to the development of subchondral sclerosis (hardening), after which the body increases the area of support due to the growth of marginal bone around the entire circumference. Joint overload leads to spondylolisthesis, which can cause compression of nerve blood vessel formations in the intervertebral discs. It is these changes that are noted in the fourth period (stage) (OP), when there is damage to the entire spinal motor segment.
Of course, any math on a clinically diverse, complex disease like the OP is pretty arbitrary. However, it can analyze clinical manifestations dependent on morphological changes, which not only allows accurate diagnosis but also identifies specific therapeutic measures.
Depending on which nerve formation, disc herniation, bone growth and other affected structures of the spine have a pathological impact, reflex and compression syndromes are distinguished.
The syndromes of lumbar osteonecrosis
Arrivecompressionincludes syndromes in which roots, blood vessels, or spinal cord are stretched, compressed, and deformed over specified vertebral structures. Arrivereflexincludes syndromes caused by the action of these structures on receptors within them, primarily the terminals of recurrent spinal nerves (Lushka's sinus nerve). The impulses transmitted along this nerve from the affected spine pass through the posterior root to the dorsal horn of the spinal cord. Switching to the anterior horns, they cause reflexive (defensive) tension of the internal muscles -reflex-tonic disorder.. Shifting to sympathetic centers of the same or adjacent lateral horns, they cause reflex vasomotor dysfunction or dystrophy. Such neurotrophic disorders occur mainly in low vascularized tissues (tendons, ligaments) at sites of attachment to bony prominences. Here, tissues undergo decomposition, swelling, they become painful, especially when stretched and palpated. In some cases, these neurotrophic disorders cause pain not only locally but also at a distance. In the second case, pain is reflected, it seems to "shoot" when touching the diseased area. Such regions are called trigger zones. Myofascial pain syndrome can occur as part of spondylolisthesis pain.. With prolonged stretching of the striated muscle, the microcirculation is disturbed in certain regions of it. Due to hypoxia and edema in the muscles, seals are formed in the form of nodules and fibers (as well as in ligaments). Pain in this case is rarely local, it does not coincide with the region of certain root growth. The reflex-myotonic syndromes include piriformis syndrome and popliteal syndrome, the characteristics of which are covered in detail in many manuals.
Arrivelocal (local) pain reflex syndromeIn lumbar osteonecrosis, low back pain is attributed to the acute development of the disease and subacute or chronic somatic pain. A critical situation is an established fact thatLumbar pain is the result of internal displacement of the nucleus pulposus. As a rule, this is a sharp pain, which often shoots through. The patient, as such, is frozen in an uncomfortable position, unable to bend over. Trying to change the position of the body increases the pain. There is complete immobilization of the lumbar region, curvature of the spine, sometimes development of scoliosis.
With hemiparesis - as a rule, pain, aggravated by movement, with axial loads. The low back can be deformed, like low back pain, but to a lesser extent.
Compression syndromes in lumbar osteonecrosis are also diverse. Among them, lens compression syndrome, tail syndrome, discoid myelopathy syndrome are distinguished.
lens compression syndromeusually develops due to disc herniation at the L . levelIV- LETSDRAWand meDRAW-Sone, because it is at this level that herniated discs are more likely to develop. Depending on the type of hernia (hernia, posterior lateral, etc. ) one or the other root is affected. As a rule, one degree corresponds to a single lesion. Clinical Manifestations of Root CompressionDRAWto the occurrence of irritation and prolapse in the skin, respectively, and the corresponding decline in muscle function.
Paresthesia(numbness, tingling) and pain spreading along the outer surface of the thigh, the anterior surface of the lower leg to the toe I. Hypalgesia may then appear in the corresponding area. In the muscles located in the L rootDRAW, especially in the anterior parts of the lower leg, atrophy and weakness develop. First, weakness is found in the extensor part of the affected finger - in the muscle that lies within the thread of the L rootDRAW. Tendon reflexes with isolated lesions of this root remain normal.
When spinal compression WILLoneirritation and shedding develop in the respective skin, extending to the area of the fifth finger. Atrophy and weakness mainly include the posterior muscles of the lower leg. The Achilles reflex decreases or disappears. Knee jerking was reduced only with the involvement of L.2, LOT3, LOTfour. Atrophy of the quadriceps, and especially the glutes, also occurs in caudal disc disease. Compression lenticular paresthesia and pain aggravated by coughing or sneezing. The pain is aggravated by movement in the lower back. There are other clinical symptoms indicating the development of root compression, their stress. The most commonly checked symptom isSymptoms of Laseguewhen you try to lift your leg up in a straight position, the pain increases sharply. An adverse variant of lumbar vertebral compression lens syndrome is cauda equilateral compression, the so-calledtail syndrome. Usually, it develops with large prolapsed medial herniated discs, when all the roots at this level are compressed. Local diagnosis is performed on the upper spine. The pain, often severe, does not spread to one leg, but as a rule, to both legs, the loss of sensitivity occupies the area of \u200b\u200 the rider's pants. With severe variants and rapid development of the syndrome, sphincter disorders are added. Lumbar myelopathy develops due to occlusion of the inferior medullary-medullary artery (usually at the base of the L . ).DRAW, ) and is manifested by weakness of the cranial, tibial, and gluteal muscle groups, sometimes with segmental sensory disturbances. Usually, ischemia develops simultaneously in the epicardial segments (L5-Sone) and a cone (S2-S5) of the spinal cord. In such cases, pelvic disorders are also involved.
In addition to the major established clinical and neurological manifestations of lumbar osteonecrosis, there are other symptoms that suggest this spinal failure. This is especially evident in the combination of disc damage against the background of congenital stenosis of the spinal canal, various malformations during the development of the spine.
Diagnosis of lumbar osteonecrosis
Diagnosis of lumbar osteonecrosisbased on the clinical picture of the disease and additional examination methods, including conventional lumbar spine X-ray, computed tomography (CT), myelogram, magnetic resonance imaging (MRI). With the introduction of spinal MRI into clinical practice, the diagnosis of lumbar osteosarcoma (PO) has been significantly improved. Cross section and Sagittal tomography allow you to see the relationship of the affected disc to surrounding tissues, including evaluation of the lumen of the spinal canal. The size, type of disc herniation, which roots are compressed, and which structures are determined. It is important to establish compliance of the leading clinical syndrome with the extent and nature of the lesion. As a rule, a patient with pinched lens syndrome will develop a mononuclear lesion and this root compression is clearly visible on MRI. This is relevant from a surgical point of view, because. this defines the active access.
Disadvantages of MRI include limitations associated with testing in patients with agoraphobia, as well as the cost of the study itself. CT is a highly informative diagnostic method, especially in combination with myelogram, but it must be remembered that the scan is performed in a horizontal plane and therefore the extent of the lesion is assumed to be correct. clinically well defined. Routine X-rays are used as a screening test and are required in the hospital. In the functional image, instability is best defined. Various bone growth abnormalities are also clearly visible on spine imaging.
Treatment of lumbar osteonecrosis
With PO, both conservative and surgical treatment are performed. Inconservative treatmentWith osteonecrosis, the following pathological conditions require treatment: orthopedic disorders, pain syndromes, impaired disc fixation, dystonia, root and marrow circulatory disorderssurvival, disturbances in neurotransmitters, changes in membrane adhesions, mental disturbances. Conservative treatments (CLs) include various chiropractic measures (immobilization, spinal traction, manual therapy), physical therapy (massage and physiotherapy, acupuncture), electrotherapy), prescription drugs. Treatment should be complex, staged. Each CL method has its own indications and contraindications, but as a rule, the general method isprescription pain relievers, non-steroidal anti-inflammatory drugs(NSAIDs),muscle relaxantandphysical therapy.
The analgesic effect is achieved with the use of diclofenac, paracetamol, tramadol. Has a pronounced pain-relieving effecta kind of medicineContains 100 mg of diclofenac sodium.
Gradual (long-term) absorption of diclofenac improves the effectiveness of therapy, prevents gastric toxic effects and makes treatment as convenient as possible for the patient (only 1-2 tablets per day). day).
If necessary, increase the daily dose of diclofenac to 150 mg, with additional analgesics in the form of long-acting tablets. In milder forms of the disease, when relatively small doses of the drug are sufficient. In the case of pain symptoms mainly at night or in the morning, the drug should be taken in the evening.
Paracetamol has less analgesic activity than other NSAIDs, and so a drug has been developed that, together with paracetamol, includes another non-opioid analgesic, propyphenazone, as well as codeine and caffeine. In patients with ischalgia pain, when using caffeine, muscle relaxation, anxiety and depression are noted. Good results have been reported with the use of the drug in the clinic for the relief of acute pain in muscle, tone and milia syndromes. According to the researchers, with short-term use, the drug is well tolerated, with practically no side effects.
NSAIDs are the most widely used drugs for PO. NSAIDs have anti-inflammatory, analgesic and antipyretic effects related to the inhibition of cyclooxygenase (COX-1 and COX-2) - an enzyme that regulates the conversion of arachidonic acid to prostaglandins, prostacyclin, thromboxane. Treatment should always begin with the appointment of the safest drugs (diclofenac, ketoprofen) at the lowest effective dose (dose-dependent side effects). In elderly patients and patients with risk factors for adverse events, treatment with meloxicam and especially with celecoxib or diclofenac/misoprostol should be initiated. Alternative routes of administration (injection, rectal) do not prevent gastrointestinal and other adverse events. The combination drug diclofenac and misoprostol has certain advantages over standard NSAIDs, helping to reduce the risk of COX-dependent side effects. In addition, misoprostol may increase the analgesic effect of diclofenac.
To eliminate the pain associated with hypertonia, it is recommended to use central muscle relaxants in complex therapy:tizanidine2-4 mg 3-4 times a day or tolperisone inside 50-100 mg 3 times a day, or intramuscular tolperisone 100 mg 2 times a day. The mechanism of action of drugs with these substances is different from that of other drugs used to reduce muscle tone. Therefore, it is used in cases where the antispasmodic effect of other drugs is not available (in so-called non-responsive cases). The advantage over other muscle relaxants used for the same indication is that with a decrease in muscle tone on the background of the appointment, there is no decrease in muscle strength. The drug is an imidazole derivative, the action of which is related to stimulation of the a . center2-adrenergic receptors. It selectively inhibits the polysynaptic component of the stretch reflex, has independent antitumor and mild anti-inflammatory effects. Tizanidine has antispasmodic effects on the spine and brain, reducing the stretch reflex and the pain caused by muscle spasms. It reduces resistance to passive movements, reduces spasms and convulsions, and increases the strength of voluntary contractions of skeletal muscles. It also has gastroprotective properties, defining its use in combination with NSAIDs. The drug has practically no side effects.
Surgerywith PO, it is done with the development of compression syndromes. It should be noted that the presence of the actual finding of a herniated disc in an MRI is not sufficient for a final decision about surgery. Up to 85% of patients with disc herniation among those have lens symptoms after conservative treatment without surgery. CL, except in some situations, should be the first step in helping patients with PO. If complex CL is not effective (within 2-3 weeks), surgical treatment (CL) is indicated in patients with disc herniation and lens symptoms.
There are urgent indications for POs. These include the development of caudal syndrome, as a rule, with complete prolapse of the disc into the lumen of the spinal canal, the development of acute hyperalgia and pronounced hyperalgic syndrome, when even theprescribed opioids, blockade does not relieve pain. It should be noted that the absolute size of the herniated disc mass is not decisive for the final decision on the operation and should be considered in conjunction with the clinical picture, the specific condition observed in the tube. tomographic survival (eg, there may be a combination of a small hernia with the background of the spinal stenosis, or vice versa - a large hernia mass that is medial to the base of the wide spinal canal).
In 95% of cases of disc herniation, the spinal canal method is used. To date, different disc puncture techniques have not been widely applied, although some authors report their effectiveness. The surgery is performed using both conventional and microsurgery instruments (with optical magnification). During the approach, the removal of the bony formations of the vertebrae is avoided using mainly intervertebral approaches. However, with narrow canals, hypertrophy of joint processes, and fixed intervertebral disc herniation, it is advisable to widen the entrance at the expense of bone structure.
The outcome of surgical treatment largely depends on the surgeon's experience and the correctness of the indications for a particular surgery. In the apt words of the famous neurosurgeon J. Brotchi, who performed more than a thousand operations for osteonecrosis, it is necessary "not to forget that the surgeon must operate on the patient. ", and not on the tomography image. "
In conclusion, I would like to emphasize once again the need for a thorough clinical examination and radiographic analysis to make an optimal decision in choosing a treatment strategy for a particular patient. .














































